Myth: Peanut allergies are a fake illness made up by hypochondriacs or foisted on children by their crazy helicopter parents.
Reality: A peanut allergy is a real and serious medical condition.
The U.S. Centers for Disease Control confirm: “Food allergies are a growing food safety and public health concern [ . . . ] Allergic reactions can be life threatening and have far-reaching effects on children and their families.” The Mayo Clinic agrees, “Even a tiny amount of the allergy-causing food can trigger signs and symptoms such as digestive problems, hives or swollen airways. In some people, a food allergy can cause severe symptoms or even a life-threatening reaction known as anaphylaxis.”
Medical tests do exist to confirm the presence of a peanut allergy or other food allergies. Depending on a person’s reported history of reaction to a food, an doctor may order a blood test, a skin prick test, or a controlled food challenge in a clinical setting to determine whether a person has a true food allergy.
Myth: There aren’t really more children with peanut allergies than there were twenty years ago. Peanut allergies are just being overdiagnosed.
Reality: Peanut allergies are genuinely on the rise among children, but scientists do not know why.
According to multiple studies published by respected groups like the U.S. Centers for Disease Control and the American Academy of Pediatrics, food allergies in general and peanut allergies in particular have increased sharply over the past few decades.
One survey study by allergists at Mount Sinai Hospital, published in the Journal of Allergy and Clinical Immunology, found that while 0.4% of children surveyed were reported to have a peanut allergy in 1997, 1.4% percent of children reported a peanut allergy in 2008 — indicating that the number of children with peanut allergies tripled in just one decade.
While it is true that occasionally blood tests or skin tests for food allergy will return a false positive result, further testing, like a medically supervised food challenge performed in a doctor’s office or hospital, can clear up confusion in the event a false positive result is suspected.
Myth: Peanut allergies aren’t that serious.
Reality: Peanut allergies put more people in the hospital every year than any other food allergy, and are the leading food-related cause of life-threatening allergic anaphylaxis.
If a person with a peanut allergy eats even a small amount of peanut protein, he or she may experience a life-threatening allergic reaction called anaphylaxis. Anaphylaxis is more than just sneezing or a few hives. Symptoms of anaphylaxis may include hives, stomach cramps, vomiting, swelling of the lips, tongue or throat, difficulty breathing, dizziness, or loss of consciousness. If left untreated, anaphylaxis can lead to a number of serious consequences including heart failure, brain damage or death.
Even people who have previously only experienced mild allergic reactions to peanuts are at risk for anaphylaxis. The severity of previous allergic reactions to a food does not reliably predict the severity of future allergic reactions to that food. For this reason, most allergists advise that all people with a known peanut allergy strictly avoid eating peanuts and carry an autoinjector filled with epineprhine, the medicine used to treat anaphylaxis.
Myth: One little bite won’t hurt.
Reality: Some people with peanut allergies react to as little as 1/100th of one peanut.
The amount of peanut protein a peanut allergic person can tolerate before suffering a reaction varies widely from person to person, but generally speaking, it is not unusual for an amount equivalent to a fraction of one peanut to cause a reaction. People on the lower end of the tolerance threshold spectrum may start showing symptoms of an allergic reaction after being exposed to as little as 1/100th of one peanut, about 5 milligrams.
This means it is absolutely possible for a person with a severe peanut allergy to have a reaction to an amount of peanut residue that cannot easily be seen, smelled or tasted. And it is one of the reasons that even people with peanut allergies who are very vigilant about avoiding foods that contain peanuts may still occasionally suffer allergic reactions from eating foods that they mistakenly, but understandably, thought would be safe.
If it seems unbelievable that even just a couple of crumbs of food could cause a severe allergic reaction, stop for a moment and consider how much venom a bee’s stinger injects. (That would be between 5 and 50 micrograms.)
Myth: If someone is suffering from a severe allergic reaction to food, you should give them Benadryl to treat it.
Reality: Epinephrine is the first-line drug of choice for a severe allergic reaction.
Benadryl (known in generic form as diphenhydramine) can provide some relief for mild allergic symptoms, like itchy skin or a stuffy nose. But the only drug known to rapidly reverse the most dangerous effects of a life-threatening anaphylactic allergic reaction is epinephrine. Epinephrine works quickly to stop two of the most dangerous symptoms of anaphylaxis: airway constriction and a sudden drop blood pressure. Benadryl does not treat those symptoms and should not be given in place of epinephrine for a severe allergic reaction. Every person with a life-threatening food allergy should get a prescription for epinephrine and should carry two epinephrine autoinjectors at all times. If you or someone you are responsible for has a life-threatening food allergy, talk to your doctor about whether Benadryl or other over-the-counter drugs should also be part of your emergency treatment plan.
Myth: Epinephrine can cause dangerous side effects so you should only use it as a last resort if you are absolutely sure a person is suffering from a very severe allergic reaction.
Reality: Epinephrine is a very safe drug and it is better to use it when not needed than to fail to use it when needed.
Epinephrine autoinjectors like the EpiPen and Auvi-Q are safe and easy to use correctly. Epinephrine, also known as adrenaline, is a hormone that occurs naturally in the human body. Serious side effects from the use of epinephrine autoinjector are extremely rare. Most reports of serious adverse health effects from epinephrine are related to accidental overdoses of IV epinephrine given in hospitals, not the use of an autoinjector. The pre-measured amount of epinephrine in an autoinjector makes it impossible to give someone an overdose with a single injection.
In fact, epinephrine is so safe and so effective that many people with severe food allergies have been advised by their doctors to use it before any symptoms arise if they realize they have accidentally eaten a food they are allergic to.
Myth: It’s impossible for a kid to get sick from just touching a peanut.
Reality: Some people with a peanut allergy develop allergic symptoms when peanuts or peanut residue touch their skin.
Some people with peanut allergies develop rashes or hives on contact when peanut residue touches their skin. Though anaphylaxis from skin contact to peanuts is thought to be rare, if peanut residue on the skin enters a person’s bloodstream through broken skin, or is inadvertently rubbed into the eyes or mouth, it could cause a more serious reaction.
Myth: It’s impossible to have an allergic reaction from peanut dust in the air.
Reality: Airborne peanut dust can cause sneezing, itchy eyes, or asthma-like symptoms in people with peanut allergies, and in rare cases, exposure to airborne peanut dust has caused anaphylaxis.
While the mere scent of peanuts has not been shown to cause allergic reactions (the aroma people associate with peanuts is not created by allergenic peanut proteins, but by other chemical compounds naturally present in peanuts), actual peanut particles in the air can cause airborne allergic reactions in people with peanut allergies. People with peanut allergies may be at risk for an airborne reaction when they are in an enclosed area where peanuts are being shelled, ground, roasted, baked or fried nearby.
Myth: It is okay for people with peanut allergies to eat peanut butter because that is not the same thing as peanuts.
Reality: Peanut butter is made from ground peanuts. People with peanut allergies need to avoid eating peanuts in all forms.
If you are shaking your head right now and asking why on Earth I included this one, GOOD FOR YOU. You get an A+ in food knowledge. However, if you happen to be a seasoned food allergy parent, you’ve almost certainly already heard from at least one well-meaning but food-unsavvy person that it ought to be all right for a person with a peanut allergy to eat peanut butter because “that’s not the same thing.”
Peanut butter is made from peanuts. Really. Check the ingredient label. it’s the first ingredient. People with peanut allergies are definitely allergic to peanut butter.
Myth: A person with a peanut allergy can eat peanut butter or peanuts safely if it’s organic peanut butter or organic peanuts.
Reality: Organic peanuts and peanut butter are just as allergenic as non-organic, conventional peanuts and peanut butter.
People with peanut allergies are allergic to peanut proteins that are present in all peanuts. All varieties of peanuts and peanut butter are unsafe for a person with a peanut allergy to eat.
(My favorite comeback to this one when I hear it in person is, “Organic peanut butter would kill my child more naturally, but he would still be dead.”)
Myth: People who are allergic to peanuts can eat peanut oil without worry, because all of the allergenic proteins have been removed.
Reality: Some types of peanut oil do contain allergenic proteins in amounts that can cause a reaction.
While it is true that highly refined peanut oil has been thoroughly processed and filtered in such a way as to remove most of the allergenic protein, much of the peanut oil sold in the United States is not highly refined oil. Less processed types of peanut oil, including cold pressed peanut oil, expelled peanut oil and crude peanut oil, have been shown to contain enough peanut protein to cause allergic reactions. Labels on peanut oil do not always reveal which type of oil is in the bottle, and food manufacturers and restaurant staff often cannot say which type they use. Therefore many allergists and food allergy organizations recommend that people with peanut allergies avoid all peanut oil.
Myth: If you cook a food thoroughly enough, any allergenic peanut protein in that food will be destroyed, making it safe for a person with a peanut allergy to eat.
Reality: The allergenic proteins in peanuts are stable in high heat, and normal cooking temperatures will not destroy them or render them safe for people with peanut allergies to eat.
It may seem like a reasonable idea: if cooking food at high temperatures can kill bacteria and viruses, won’t it “kill” peanut proteins, too? But allergenic peanut proteins aren’t alive; they can’t be “killed” by heat. In fact, some studies have actually shown that roasting peanuts makes them more allergenic, not less.
While food proteins cannot be “killed” by heat since they were never alive in the first place, it is actually true that some food proteins do change shape when exposed to heat, and this can actually make certain common food allergens less allergenic. Eggs are a good example of a food that becomes less allergenic when heated. A protein called albumin in eggs changes shape when heated; this is why eggs turn from a liquid to a solid when you cook them. Because allergic reactions are triggered by proteins with a specific shape, the change in the shape of the albumin in cooked eggs makes it less allergenic. So some people who are allergic to egg albumin are able to eat eggs that have been thoroughly cooked. It is also true that some people with milk allergies are able to safely eat cooked foods that contain milk even though they would have an allergic reaction to uncooked dairy products.
But the proteins that cause peanut allergies do not change shape at normal cooking temperatures. So you cannot make a food that contains peanuts or has been exposed to peanut residue safe for a person with a peanut allergy by thoroughly cooking it.
Myth: If you just brush the peanut topping off of a cake, scrape the nuts off a cheese ball, or pick the peanuts out of a salad, that will make the food safe for a person with a peanut allergy to eat.
Reality: Even if you remove visible nuts from a dish, trace amounts of peanut protein might remain. And even very trace amounts of peanut protein can cause an allergic reaction in a person with a peanut allergy.
As mentioned above, less than 1/100th of one peanut can cause allergic symptoms in highly sensitive people. Once peanuts or peanut butter have directly touched a food, that food should no longer be considered safe for a person with a life-threatening peanut allergy to eat.
Myth: Hand sanitizer will remove peanut protein from hands.
Reality: Hand sanitizer does not remove or destroy peanut protein. To effectively remove peanut residue you must wash your hands with soap and water, or use a wet wipe.
Hand sanitizers may kill viruses and bacteria, but all they do to allergenic peanut residue is spread it around. The most effective way to remove peanut residue from your hands is to wash them well with soap and water. If soap and water are not available, wet wipes made for handwashing have also been shown to be effective at removing peanut residue.
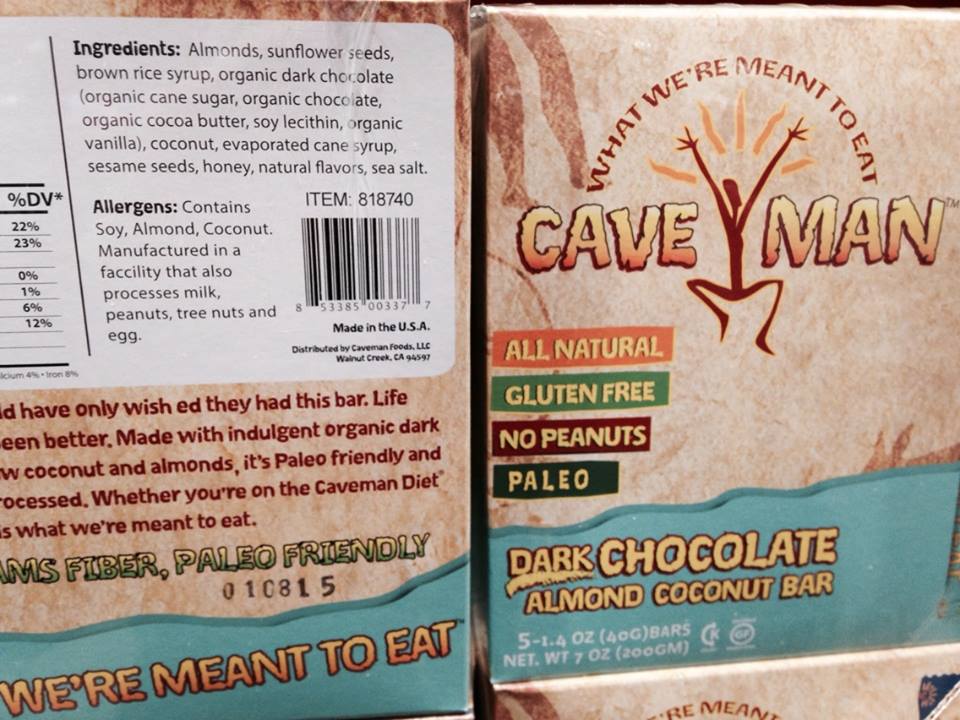
Myth: Food companies in the U.S. are required to put warning labels on food packaging if there is any chance that the food might contain traces of peanuts.
Reality: Allergen advisory labels like “may contain peanuts” or “made on shared equipment with peanuts” are voluntary and unregulated by U.S. law. Food companies are not required to use them.
The Food Allergen Labeling and Consumer Protection Act (FALCPA) requires that food companies list the top 8 most common food allergens– milk, eggs, wheat, soy, fish, shellfish, tree nuts and peanuts– in clear language on labels if they are intentional ingredients. So, for example, a granola bar that contains peanut flour as an ingredient must say on the label that it contains peanuts or peanut flour; the company that makes the granola bar is not allowed to call peanut flour something vague like “vegetable protein flour” or “natural flavoring.”
However, the FALCPA law only applies to packaged foods regulated by the U.S. Food and Drug Administration. It does not apply to foods regulated by the U.S. Department of Agriculture, like fresh meat, eggs and cheese. And FALCPA does not require that companies put an allergen advisory warning on products that may contain top 8 allergens by accident. For example: if an ice cream manufacturer runs peanut butter ice cream through its ice cream making machine and then runs chocolate ice cream through the same machine immediately afterward, that company would not be required to put a warning label on the chocolate ice cream to let customers know that it may contain traces of peanuts.
When companies choose to add labels like “May contain peanuts,” “Made on shared equipment with peanuts,” or “Made in a shared facility with peanuts,” they are doing so voluntarily. If a product does not have an allergen advisory warning for peanuts, that does not mean that the product is definitely peanut-free.
Myth: If a food product says “No Nuts,” “Nut-free” or “Peanut-free” on the package, that definitely means it was made in a peanut-free facility.
Reality: The U.S. government does not regulate “Nut-free” or “Peanut-free” labeling on food packaging.
It is perfectly legal for a food company to print “Peanut-free” on the front of a label and “Made on shared equipment with peanuts” on the back, and yes, I HAVE SEEN LABELS LIKE THAT IN REAL LIFE.
No, really.