Once upon a time, people living with life-threatening allergies in the United States had basically one choice for an epinephrine autojector: the EpiPen.
First approved for sale to patients by the FDA in the 1980s, and redesigned to be slightly more user-friendly in 2009, the EpiPen opened the market for epinephrine autoinjectors, and dominated it for the next thirty years.
Before the EpiPen, to self-administer epinephrine during a severe allergic reaction, people with life-threatening allergies to food, insects, or medications relied on cumbersome syringes and vials– which were fragile, challenging to carry in a purse or pocket, and even more challenging to use correctly and quickly when anaphylaxis symptoms struck. For people who were accustomed to fumbling with fragile pre-filled syringes, or, worse, trying to draw up a correct dose with a sharp needle and a glass vial during a reaction, the rugged, simple-to-use EpiPen autoinjector was an amazing improvement.
Since its debut, the EpiPen has become one of those brand names– like Band-Aid, Tylenol, or Kleenex– that is almost synonymous with the type of product it represents. To many people, just as a small self-adhesive bandage is simply called Band-Aid, an epinephrine autoinjector is called an EpiPen.
But in recent years, a number of new types of epinephrine autoinjectors have become available to patients. And, even as brand-name EpiPen prices have skyrocketed over the past decade, manufacturing problems with the EpiPen have caused recalls and shortages of the device.
Is the old standby, brand-name EpiPen really still the best option among EAIs? Or would one of these EpiPen alternatives– which contain exactly the same type of injectable epinephrine as an EpiPen, but in some cases, use a different injector design– work better for you? Here is a breakdown of different epinephrine delivery options to help you decide:
The EpiPen
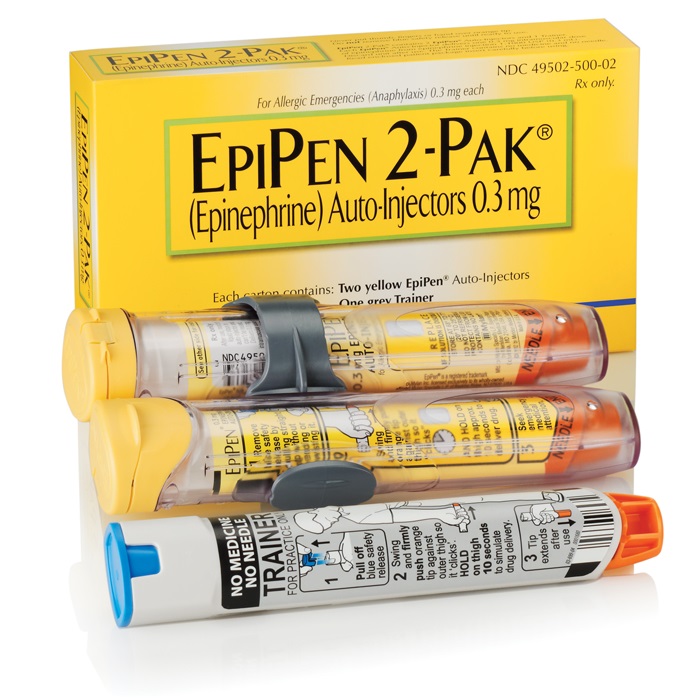
The Pros:
High prices and ongoing EpiPen shortages have many patients who have used the EpiPen for years considering a switch to a different epinephrine delivery option. But the classic autoinjector has a few important things going for it:
Lots of people with allergies already know how to use the EpiPen.
For those who are already well-trained on how to use the EpiPen, the idea of switching to a different device, with different directions, might be frustrating. This might be especially true for small children. If you’ve already spent a year diligently training your easily-distracted, needle-phobic five-year-old to self-carry and self-inject an EpiPen, convincing the kid to switch to an entirely different device might feel like a challenge.
Lots of people who don’t have allergies already know how to use EpiPens, too.
School nurses, teachers, childcare providers, EMTs, and other people who train to administer epinephrine autoinjectors on others as part of basic first aid or job training are often first taught with brand-name EpiPen training devices and materials. If you choose to use a different style of EAI, you might find that you need to retrain caregivers, colleagues, family, or friends.
The EpiPen has safety features some other EAIs don’t have.
The 2009 redesign of the EpiPen equipped it with a few safety features that many users appreciate. First, the EpiPen’s color coded top and bottom ends (blue to the sky, orange to the thigh) help to prevent users from using the device upside-down and accidentally injecting themselves in a finger or thumb instead of properly injecting themselves or another person in the thigh.
Second, a pop-out needle cover automatically engages after the EpiPen is fired, protecting the user and bystanders from any unplanned encounters with a used needle by completely enclosing it. This feature can be especially reassuring in daycare or school settings.
The Cons:
EpiPens are expensive.
Anyone who has had to pay the list price can tell you: EpiPens cost several hundred dollars. The price for the brand name device is so high that many insurance companies have started limiting the number of brand name EpiPen sets they will cover within a certain timeframe, or have entirely stopped covering them. And if you have a high deductible plan, even if your insurance technically covers the EpiPen, you may face some serious sticker shock when it comes time to pick up that prescription.
EpiPen shortages keep happening.
Mylan, the EpiPen maker, has suffered repeat production and supply problems over the past few years, and rolling shortages nationwide have meant many pharmacies simply can’t keep brand name EpiPens in stock.
This ongoing access issue has been much more than an annoyance for people who rely on epinephrine as a life-saving medication. The shortages haven’t just caused people with life-threatening allergies temporary difficulties in accessing their medication– they have also caused many people who have been loyal EpiPen users for years to lose trust in Mylan as a company.
The old standby is, well, old.
The EpiPen’s design hasn’t changed in ten years, and while the 2009 redesign did introduce a few nice new features like the automatic needle cover, the basic shape and underlying mechanism are very similar to the original EpiPen designed in the 1980s.
While this means you are getting a familiar, time-tested device in an EpiPen, it also means you won’t be getting newer EAI features, like the recorded audio instructions offered by the Auvi-Q.
Learn how to use an EpiPen brand epinephrine autoinjector at the EpiPen website.
The Mylan Generic
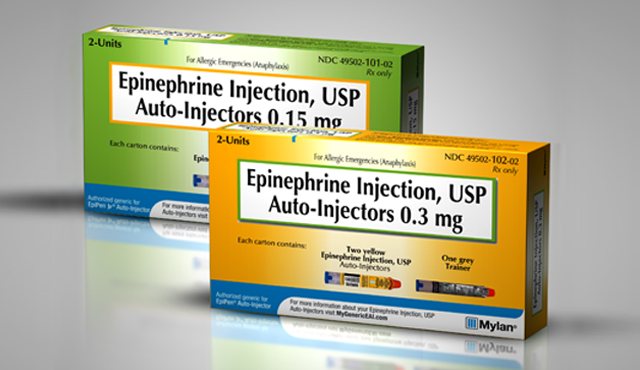
The Pros:
Do you wish you could buy an autoinjector that was just like an EpiPen, but less expensive? If so, the Mylan generic EAI is the probably right device for you.
It’s the EpiPen you recognize, in a plain wrapper.
The Mylan generic epinephrine autoinjector is made by the same company that makes the EpiPen. It has the same design as the post-2009 brand name EpiPen, comes with the same directions, and contains the same medication in the same formulation.
The Mylan generic is less expensive than the brand name EpiPen.
Did we mention already that the brand name EpiPen is really expensive? Like, as in, Congress investigated EpiPen maker Mylan for price gouging expensive?
The Mylan generic EAI retails for about half the price of Mylan’s brand name device.
The Cons:
It’s the EpiPen you recognize, in a plain wrapper– and maybe that’s actually not what you want.
The Mylan generic autoinjector has the same design as the brand name EpiPen– which means it has the same design-based limitations mentioned for the EpiPen above. If you are looking for innovative EAI features like a retracting needle or audio cues, you will not find them here.
It is less expensive than the EpiPen, but it may NOT be your least expensive option.
Patient costs for different EAIs can vary depending on your region, your pharmacy, and your insurance plan. But the Adrenaclick generic epinephrine autoinjector often costs less than the Mylan generic EAI.
Learn more about the Mylan generic epinephrine autoinjector at the Mylan generic website. (Note: the user directions are the same as for the EpiPen above.)
The Adrenaclick

The Pros:
It’s time-tested: the Adrenaclick EAI has been around longer than you might think.
If one of your worries about trying a new-to-you style of epinephrine injector is that the product might not have been around long yet enough for design flaws to be revealed, you can set that concern aside with the Adrenaclick by Amedra.
The Adrenaclick brand epinephrine autoinjector first hit the market, with its current design, in 2009. Due to distribution issues, production delays, company buyouts and mergers (six different companies have owned the rights to produce the brand name Adrenaclick since it was invented!) and a brief discontinuation of the product back in 2012, the Adrenaclick has never been as well-marketed, as well-known, or as widely-used as its competitors.
But the Adrenaclick’s basic design– which is actually not that different from the design the original EpiPen had before its redesign– has remained the same for nearly a decade. That means lots of patients have used the Adrenaclick successfully– and continue to trust it.
The Cons:
The Adrenaclick lacks key features that other epinephrine autoinjectors offer.
The EpiPen and the Auvi-Q each require the user to remove one safety cap in order to inject epinephrine. The Adrenaclick design requires that the user remove two caps– one from each end of the device. That makes the user instructions slightly more complicated than those for the EpiPen or Auvi-Q– which can matter when a person who is trying to self-administer epinephrine is disoriented due to anaphylaxis symptoms, or when an untrained bystander is trying to figure out how to use the EAI.
The Adrenaclick also lacks an important safety feature that other EAIs offer. The EpiPen and Auvi-Q both have a mechanism in place to automatically cover the needle after an injection. The EpiPen uses an automatic pop-out needle cover; the Auvi-Q, a retracting needle. But the Adrenaclick needle is left exposed after use, and must be manually covered by carefully placing the device back in its carrying case after use.
The Adrenaclick doesn’t come packaged with a trainer.
Unlike the EpiPen or Auvi-Q, a free trainer is not included in every Adrenaclick package. Instead, you have to order a trainer separately through the mail.
This is a serious disadvantage for people who need to learn how to use an epinephrine autoinjector right away because they are newly diagnosed, or because they are new to the Adrenaclick and do not have a backup supply of a more familiar EAI available to use until the trainer comes.
Its unpopularity means bystanders, caregivers, and medical professionals may not have seen an Adrenaclick before and may not know how to use it.
This is an issue with ANY autoinjector. But Teva’s EAI design is less different from an EpiPen than the Adrenaclick design is, and the Auvi-Q offers recorded instructions that play automatically when you use the device, that can walk an untrained person through the injection process. Someone who has not been previously trained on how to use the Adrenaclick autoinjector would have to consult the product packaging to figure out how to use one in an emergency.
If you do decide to switch from an EpiPen to an Adrenaclick, make sure that any friends, family, caregivers, coworkers, teachers, etc. who might need to help treat an allergic reaction with the Adrenaclick have get trained on how to use one, if they have not already learned.
The brand name Adrenaclick may not cost you any less than the Mylan generic.
Depending on what coverage your insurance offers and which pharmacy you use, the brand name version of the Adrenaclick may actually cost you more than the Mylan generic. But the makers of the Adrenaclick offer a second EAI option which, depending on where and how you buy it, may be much cheaper than either: the Adrenaclick generic, explored below.
Learn how to use the Adrenaclick epinephrine autoinjector at the Adrenaclick website.
The Adrenaclick Generic

Note: some refer to this generic EAI as “the Impax generic” after the company that makes it, or “the CVS generic” because CVS pharmacies offer it preferentially over other generic EAIs.
The Pros:
It has all the same features as the brand name Adrenaclick, except for the branding. But it costs less.
The Adrenaclick generic offers all of the features of the regular Adrenaclick: the same time-tested design, with the same medication inside. But its retail price is much lower than the brand name Adrenaclick.
The Adrenaclick generic might be the least expensive EAI option for you.
Depending on your pharmacy and insurance options, the Adrenaclick generic epinephrine autoinjector may be the cheapest EAI you can buy in the United States.
Some pharmacies offer this generic autoinjector for as low as $100 for a two-pack.
Other pros are the same as those listed for the brand name Adrenaclick.
The Cons:
See the cons list for the brand name Adrenaclick above. They are the same, except for the price for the Adrenaclick generic, which as noted above is quite low compared to other EAIs.
The Auvi-Q

The Pros:
The Auvi-Q offers a unique set of user-friendly features different from any other epinephrine autoinjector on the market.
The Auvi-Q was actually designed by people with food allergies to be a more user-friendly EAI option. The Auvi-Q inventors, who grew up carrying (and sometimes forgetting) their own EpiPens, set out to create a device that would be both more convenient to carry and easier to use than an EpiPen. If you are looking for the autoinjector with the most innovative, user-friendly features, the Auvi-Q is definitely the EAI you want in your pocket.
Speaking of which . . .
The Auvi-Q will fit in your pocket. Really.
Unlike the tube-shaped EpiPen, Teva, or Adrenaclick, or their generic dopplegangers, the Auvi-Q will actually fit in most normal-sized pants pockets comfortably. It is roughly the size and shape of a small cell phone or wallet– making it the ideal option to slip discreetly into a jeans pocket or a small purse.
An Auvi-Q will tell you, or a bystander, how to inject epinephrine, out loud.
In addition to printed directions that appear on the device (similar to the directions printed on other autoinjectors), the Auvi-Q offers automatic, recorded step-by-step voice instructions that walk a user through using the device properly during an allergic reaction. (That’s actually where the Auvi-Q name comes from: the autoinjector has both “audio” and “visual” cues: au + vi + qs. Get it?)
Auvi-Qs feature a retracting needle.
A retracting needle that automatically snaps back into the device after use, to protect the user and bystanders from accidental needle injuries. This is a similar feature to the EpiPen’s pop-out needle cover, and is an advantage over the Adrenaclick or Adrenaclick generic.
Auvi-Q is the only epinephrine autoinjector that offers a dose sized for babies.
Maker kaléo recently designed a new version of the Auvi-Q that contains the correct dose of epinephrine for infants and toddlers weighing 16.5 – 33 pounds. No other EAI on the market in the U.S. offers this option. Up to this point, parents, caregivers and health care providers, when faced with an infant or toddler who was suffering a life-threatening allergic reaction, but was under the 33 pound weight minimum for “junior” epinephrine autoinjectors, could only choose between treating a reaction with a cumbersome needle and syringe, or with devices designed and dosed for older children.
You may be able to get Auvi-Qs for free through Auvi-Q maker kaléo’s zero co-pay program.
If you have private commercial health insurance, but your insurance does not cover the Auvi-Q, you may be qualify to receive a set of Auvi-Q autoinjectors for free from the manufacturer. Various restrictions apply to this offer; contact kaléo for details.
The Cons:
Auvi-Q is only available by mail-order, or at certain Walgreens locations.
Auvi-Qs are probably not available at your corner pharmacy. Currently, the only way to get an Auvi-Q set is to ask your doctor to contact the Auvi-Q manufacturer, kaléo, and ask to set up mail delivery through one of the mail order pharmacies kaléo partners with, or arrange to pick your set up at a participating Walgreens– which is the only brick-and-mortar pharmacy that carries the Auvi-Q, and which, according the to Auvi-Q website’s FAQ, only allows in-store pickup of Auvi-Qs for those whose insurance covers it; participants in Auvi-Qs zero copay or affordability programs must still use a mail-order pharmacy.
This means, firstly, that your prescribing doctor has to be familiar with the Auvi-Q ordering process in order for you to get one. Secondly, if you do take delivery by mail (which is the most common way to get an Auvi-Q) you will have to deal with the typical issues associated with the delivery of mail order medications: delivery can take several days, and there is some chance that your package of live-saving medicine might wind up rain-soaked, overheated, smashed, taken by porch pirates, delivered to the wrong house, etc.
For patients who need access to epinephrine autoinjectors immediately– because they are newly diagnosed, because they used their entire supply to treat a reaction, because a school or daycare is demanding a new set for the office, etc., the delay and potential logistical issues associated with mail-order might be a dealbreaker. But you may be able to get around this problem if you are able to pick your prescription up at a Walgreens that has Auvi-Qs in stock.
Your insurance may not cover Auvi-Q. And the list price is very expensive.
Auvi-Q maker kaléo has come under some criticism for its complicated pricing system– which lists an insurance company price of several thousand dollars per set that many insurance companies simply refuse to pay.
Patients are basically never asked to pay the insurance company price for the Auvi-Q, though. Many patients whose insurance companies will not cover the Auvi-Q qualify for the zero copay plan mentioned above; others may qualify for kaléo’s patient assistance program for low-income households. And the cash price that kaléo charges patients who want to purchase the device directly is significantly lower than the insurance company price– more in line with the cost of other EAIs like the Adrenaclick or the Mylan generic.
If, as a patient, you do ever get quoted an exorbitant price in the several thousand dollar range for an Auvi-Q by an insurance company, doctor, or pharmacy, make sure to check directly with kaléo to make sure you are not missing out on one of their discount programs.
Auvi-Q is not as familiar to the public as the EpiPen.
Like the Adrenaclick, the Auvi-Q is both newer to the market and less popular than the EpiPen, which means that healthcare providers, caregivers, school staff, etc., who may have already been trained to use EpiPens, might not be familiar with the Auvi-Q and might not know how to use it.
While this is technically a disadvantage, the Auvi-Q’s voice instructions theoretically make it the easiest epinephrine autoinjector for an untrained bystander to use correctly (assuming they can hear and understand instructions in English). And as the Auvi-Q has become more popular and more widely advertised, lack of public familiarity with the device has become less of an issue.
Learn how to use the Auvi-Q epinephrine autoinjector at the Auvi-Q website.
The Teva Generic

The Pros:
Teva’s EAI is a lot like the brand name EpiPen you may already be used to.
The Teva generic epinephrine autoinjector contains the same active ingredient as the classic EpiPen: epinephrine. And it’s available in the same adult and junior dose sizes as an EpiPen. The shape and style of the autoinjector are also similar in many ways to an EpiPen, but, the two-cap design, involving a sealed twist cap at the bottom of the device, means the usage directions are slightly different.
The Teva generic costs less than a brand name EpiPen
The Teva generic is priced a couple of hundred dollars lower than Mylan’s brand name device.
The Cons:
The Teva generic is just different enough from the EpiPen to be potentially confusing.
The Teva generic looks very similar to an EpiPen– moreso than any other device on this list besides Mylan’s own generic. But the directions for use are just different enough that they could cause a delay in someone using the medication properly if they mistook the Teva device for a more familiar EpiPen or Mylan generic.
The Teva generic is not less expensive than the Mylan generic, and may cost more than the Adrenaclick generic.
Teva’s generic version of the EpiPen costs about the same as Mylan’s generic. At that price, it might not make sense for someone who has already been trained to use an EpiPen to switch to a new autoinjector with different instructions– unless the EpiPen and Mylan generic are both unavailable locally due to Mylan’s ongoing shortage issues.
Teva seems to have its own EAI shortage problems.
Teva received approval from the FDA to start selling its generic epinephrine autoinjector back in 2018, but, by mid-2019, the company had still not made the device widely available at pharmacies. Teva has been slow to ramp up production of their autoinjector to meet demand, even with ongoing EpiPen and Mylan generic shortages providing Teva with what should be a prime opportunity to find some new customers.
Learn how to use the Teva generic epinephrine autoinjector at the Teva website.
The Symjepi Syringe

Note: it’s important to state that the latest epinephrine delivery device on the U.S. market, which just became available directly to patients in mid-2019, is not an epinephrine autoinjector.
The Symjepi is a pre-filled syringe, not really that unlike the single-dose, pre-filled syringes many people with life-threatening allergies used to carry before the EpiPen became available. The key difference between the Symjepi syringe and the old school pre-filled epinephrine syringe kit your grandmother might have used is that the Symjepi is made of a rugged plastic material and comes with a needle cap and a hard plastic carrying case. This design makes the Symjepi less likely to break than a standard pre-filled syringe, and the opaque syringe and case also protect the epinephrine inside from light exposure, which is important, since epinephrine quality can be degraded by repeat exposure to light.
Because the Symjepi syringe is not actually an epinephrine autoinjector, it’s not exactly in the same category as the devices above, and should not be considered a one-to-one replacement for someone who currently carries EAIs. But the Symjepi may meet the specific needs of some people with life-threatening allergies, perhaps especially as a backup option, which is why I will include some pros and cons for it here.
The Pros:
The Symjepi syringe is smaller than an epinephrine autoinjector.
Because it does not contain an autoinjection mechanism, the Symjepi syringe is smaller than an autoinjector. This means it should easily fit into a pocket or purse. It also means it would take up less space in a medicine cabinet or portable first aid kit.
The Symjepi features a post-injection needle cover.
Nothing about the Symjepi is automatic; it is a fully manual device. So the needle cover on the Symjepi does not pop out automatically after use like it does on the EpiPen and Mylan generic autoinjectors. But the Symjepi does feature an integrated needle cover that the user can physically pull out to cover the needle after use.
The Symjepi is less expensive than some autoinjector options.
Priced under $300, the Symjepi is definitely cheaper than a brand-name EpiPen, and also is less expensive than the typical patient cash price for an Auvi-Q. However, it is comparable price-wise to some of the generic epinephrine autoinjector options, so depending on insurance coverage and local pricing, it may not be the cheapest option for you.
The Cons:
The Symjepi is more complicated to use than an autoinjector.
The Symjepi device is a syringe. To use it, you must remove the needle cap to expose the needle, inject the needle into the thigh at the correct location and angle, and then depress the plunger to dispense the medicine inside. This might not seem like a very complicated set of directions, but consider how it differs from an autoinjector:
- When you use an autoinjector, the plastic base of the device helps stabilize it against the thigh before the needle is released, making it easier to insert the needle at the correct angle. With the Symjepi, you uncover the entire needle when you remove the cap, and must judge the correct insertion angle for yourself.
- You must remember to insert the needle first and then push the plunger second. If you accidentally push down on the plunger at all before inserting the needle, some or all of the epinephrine will leak out of the needle end of the syringe before you can inject it into the thigh.
These differences could make it difficult for a person who is disoriented from anaphylaxis symptoms (which commonly include dizziness, confusion, and shortness of breath) to use the Symjepi properly. The Symjepi would also likely be more difficult for a small child to use than an autoinjector.
Adults with some basic experience using other types of syringes to inject medication may feel quite comfortable using the Symjepi, though, especially if they are not planning to use it to inject themselves during anaphylaxis, but instead, planning to use it to treat another person with an allergy. It could be a good option for school nurses to keep stocked in their offices, or for EMTs to carry on ambulances, in place of bulkier or more expensive options.
The Symjepi is not significantly less expensive than autoinjectors with more user-friendly directions and better safety features.
A patient who can get an Auvi-Q — with a convenient wallet-shaped profile, a retracting needle and voice instructions — for free through kaléo’s zero copay program, or who can get an Adrenaclick generic autoinjector for, say, $250 at their local pharmacy, is probably not going to want to pay $280 or so for what is essentially a beefed up version of the pre-EpiPen era pre-filled syringe.
If Symjepi manufacturer Adamis does not lower the price of their epinephrine syringe to offer a significant savings in comparison with generic epinephrine autoinjectors, they may struggle to compete with the other devices already on the market that offer more features.
Learn how to use the Symjepi epinephrine syringe at the Symjepi website.
Featured epinephrine autoinjector photo by Tony Webster, used under Creative Commons license.
















